 |
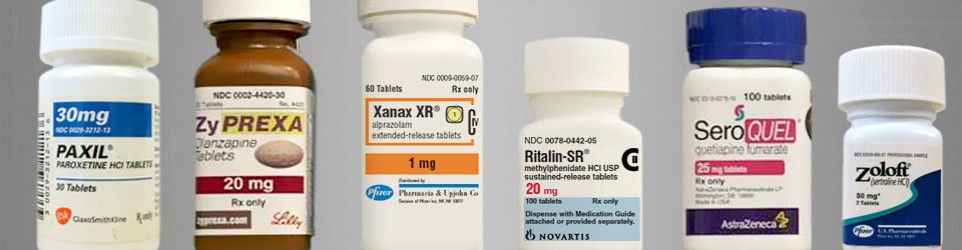
| When are all the new drugs for psychiatric disorders coming along? Probably not in your lifetime. |
Schizophrenia Bulletin, Fibiger (2012)
"Psychopharmacology is in crisis. The data are in, and it is clear that a massive experiment has failed: despite decades of research and billions of dollars invested, not a single mechanistically novel drug has reached the psychiatric market in more than 30 years. Indeed, despite enormous effort, the field has not been able to escape the “me too/me (questionably) better” straightjacket. In recent years, the appreciation of this reality has had profound consequences for innovation in psychopharmacology because nearly every major pharmaceutical company has either reduced greatly or abandoned research and development of mechanistically novel psychiatric drugs. This decision is understandable because pharmaceutical and biotechnology executives see less risky opportunities in other therapeutic areas, cancer and immunology being the current pipeline favorites. Indeed, in retrospect, one can wonder why it took so long for industry to abandon psychiatry therapeutics. So how did we get here and more importantly, what do we need to do to find a way forward?
The discovery of all three major classes of psychiatric drugs, antidepressants, antipsychotics, and anxiolytics, came about on the basis of serendipitous clinical observation. [Also known as dumb luck.] At the time of their discoveries, the mechanisms by which these molecules produce their effects were unknown, and it was only later that antipsychotics were shown to be D2 receptor antagonists, antidepressants monoamine reuptake inhibitors, and anxiolytics GABA receptor modulators. It is interesting and perhaps instructive to consider whether any of these classes of drugs could have been discovered by current drug discovery strategies. For example, what genetic or preclinical data exist that point to the D2 dopamine receptor as a likely target for antipsychotic activity? Presently there are no genetic data that suggest that this receptor is expressed or functions abnormally in psychotic disorders. And without the benefit of the prior clinical validation, it is difficult to see how preclinical data alone would point to the D2 receptor as an interesting potential target for the treatment of psychotic disorders. The same can be said for monoamine transporters with respect to depression where, like psychosis, there are no animal models based on disease pathophysiology and no compelling preclinical data pointing to these as potential targets for antidepressant drugs. This raises a troubling question: if in retrospect the three major classes of currently prescribed psychiatric drugs would likely never have been discovered using current drug discovery strategies, why should we believe that such strategies are likely to bear fruit now or in the future?
In order to recapture industry’s investment in psychiatric drug development, major changes in psychiatry will need to take place. These changes are necessary along the entire value chain, including both preclinical and clinical domains. What the field lacks is sufficient basic knowledge about normal brain function and how its disturbance underlies the pathophysiology of psychiatric disease. Because of this, as the record now clearly shows, it remains too early to attempt rational drug design for psychiatric diseases as currently conceived. The most obvious solution here is expanded investment in neuroscience. By necessity, this will be driven primarily by the efforts of clinical and basic scientists in academic settings because industry no longer has the appetite or the resources to engage in such activities. It is worth emphasizing that industry is in the business of making drugs, knowledge sometimes being a fortuitous byproduct. Academia is in the business of generating knowledge, and knowledge is what is needed at present. If we are successful in making the necessary changes, given the enormous level of unmet need left by existing psychiatric drugs, there is no doubt that industry will return and reinvest.
A major barrier to progress is the current state of nosology in psychiatry. A new taxonomy is a prerequisite for meaningful progress. Today, few would argue that syndromes such as schizophrenia and depression are single, homogeneous diseases. And yet when it comes to clinical research, including clinical trials, both are still almost always treated as such. For example, studies continue to be published on the genetics of both of these syndromes despite the fact that there never will be a robust genetics of either condition as the nature and severity of specific symptoms are too heterogeneous across individuals to have any consistent genetic correlates. Similarly, while DSM conceptualizations of psychiatric disease may have utility in current clinical practice, when it comes to research, they too are a barrier to progress. A different approach would be to break these syndromes down into their component subsyndromes or symptoms and investigate the neurobiological substrates of these more precisely defined components. As an example, although there will never be a coherent biology of schizophrenia (any more than there ever could have been be a meaningful biology of cancer as it was understood 30 years ago), the chances seem better that there will be a biology of subsyndromes such as negative symptoms, delusions, or hallucinations (just as it is now understood that there are distinct biologies underlying different cancers). Advances in knowledge about the biological mechanisms underlying different cancers are were a prerequisite for the huge current investment in developing novel cancer therapeutics. Psychiatry should learn from this example.
Given that there cannot be a coherent biology for syndromes as heterogeneous as schizophrenia, it is not surprising that the field has failed to validate distinct molecular targets for the purpose of developing mechanistically novel therapeutics."






