 |
| It's amazing what clinicians will do just to avoid entering into a therapeutic relationship with their suicidal patients (especially the borderlines). I really wish they had a control condition in which the hospitalized suicidal patients had daily individual sessions with an empathic therapist (the same therapist they would get to see on a weekly basis after their release). This study would have to replicated, of course. And we should keep in mind that there are other ways to reduce pain and suicidal ideation that don't involve drugs, such as building physical endurance in high-risk suicidal patients through mountain hiking. Seriously, check it out. |
Scientific American
"Could mental pain be treated like physical pain, and would a reduction in suicidal thoughts follow? A surprising new study by Yovell and colleagues in Israel addressed that question in a randomized, placebo-controlled trial of very low doses of an opioid, buprenorphine, in severely suicidal subjects.
The authors looked to the concept of “separation distress” to justify the trial of buprenorphine. All young animals, including humans, are distressed when separated from the attachment figures on whom their physical and emotional well-being depends. Very low doses of opioids have been known to ameliorate that distress since the 1970s. The authors of the current study drew on attachment literature which established that endogenous opioids—the ones that occur naturally in our brains—help us feel good when we are with loved ones. When we separate from loved ones, internal opioid levels drop, and we experience mental pain—the human version of separation distress.
Neurobiological studies have suggested that separation distress overlaps with pain circuitry in the brain in a general “neural alarm system” when an animal, or a person, is under threat. A trial of opioid painkillers, which might quiet that neural alarm system, seemed reasonable.
It was also necessary. There are currently no medications to quickly relieve suicidal thoughts. Antidepressants can take a month or longer to ease depression, and many psychiatrists today, like Shneidman, believe that depression and suicidal ideation are separate conditions. Treating depression might not even address suicidal thinking. A medication that specifically targets suicidal ideation—quickly—could be lifesaving.
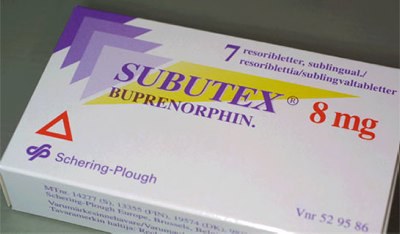
Buprenorphine, sold as Subutex in pure form and as Suboxone when combined with naloxone (which decreases its abuse potential) is an unusual opioid in that it stimulates some, but not all, of the brain’s opioid receptors. It causes less euphoria than opioids like hydrocodone, the active ingredient in Vicodin, and hydromorphone, the active ingredient in Dilaudid, but relieves pain and withdrawal symptoms; in fact, it was developed as a treatment for opioid addiction. Because it is less pleasurable, it is less likely to be abused, and because it is weaker, it is safer in overdose. Individuals who do abuse buprenorphine get high by crushing the tablets and injecting a solution made from the powder. The investigators used a gelatin-based lozenge that dissolves under the tongue to make that impossible.
Yovell and colleagues recruited patients from four hospitals in Israel and assigned them to receive tiny doses of buprenorphine or placebo. At the outset, the subjects were quite ill; the majority had made suicide attempts in the past, and 57% met criteria for borderline personality disorder, which is characterized by chronic suicidal ideation and rejection-sensitivity—meaning that mild slights can cause their mood to plunge. The Beck Scale for Suicide Ideation was used to rate patients’ suicidality before, during, and after the intervention.
The authors found a significant drop in suicidal thinking in the buprenorphine group versus the placebo group. Buprenorphine had a positive effect on depression, but the impact on suicidal thinking was even greater. Further, patients who met criteria for borderline personality disorder benefited even more than patients with depression alone. For the investigators, this finding closed a loop: extreme distress over real or perceived abandonment is a hallmark of borderline personality disorder. In borderline patients, suicidal thoughts may emerge when their highly sensitive separation distress systems are activated, with a drop in endogenous opioids and subsequent mental pain. The robust improvements in suicidal ideation in borderline patients suggested that buprenorphine treats the psychache associated with abandonment and rejection.
The study could not prove that opioids treat mental pain—it wasn’t designed to do so—but it did show that buprenorphine decreases suicidal ideation. Perhaps the study’s most important contribution is its implication that treatments that help us withstand mental pain may prevent suicide."
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.